Source: Centers for Medicare & Medicaid Services
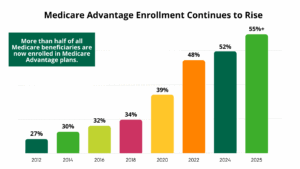
As Medicare Advantage (MA) continues its steady rise — now covering over 55% of all Medicare beneficiaries — healthcare organizations face a pressing challenge: how to retain MA patients within their networks and reduce revenue-draining referral leakage. In an increasingly value-driven healthcare environment, understanding the flow of MA patients across care settings is not just a matter of operational efficiency; it’s a strategic imperative.
Referral leakage, when left unchecked, fragments patient care and weakens relationships across the continuum. But with access to the right data — specifically, granular, timely insights into referral behavior and patient movement — health systems, ACOs, and post-acute providers can begin to reverse this trend.
The Hidden Cost of Referral Leakage in MA
Referral leakage is not always obvious, but its impact is substantial. When MA patients are referred outside the preferred or affiliated network, organizations risk:
- Losing control over patient outcomes and care coordination
- Missing opportunities to align with value-based contract goals
- Sacrificing revenue and downstream utilization to competing providers
As MA becomes the default path for the majority of Medicare beneficiaries, reducing leakage is no longer optional. Providers must understand not only where patients are going but also why they are leaving.
Following the Flow: Understanding Where Patients Go
One of the most effective ways to reduce leakage is to analyze the pathways patients take after a referral — especially those who exit the network. Claims-based data enables organizations to track:
- Referral destinations by provider, facility, and geography
- Out-of-network usage rates by specialty
- Shifts in patient movement over time
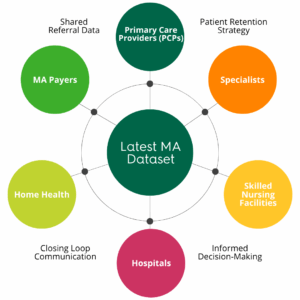
Access to payer-level referral intelligence enables organizations to see not only where MA patients are going, but which payers are facilitating those transitions. This level of granularity helps leaders identify emerging referral patterns and pinpoint key leakage sources across hospitals, physicians, and post-acute providers.
Tools for Visualization and Monitoring
Data alone is not enough. To drive strategic decisions, organizations must be able to visualize and interpret referral trends in real time.
Modern analytics platforms now offer dynamic dashboards that:
- Highlight leakage hotspots across specific service lines or locations
- Compare referral performance over time and across competitors
- Surface underutilized or untapped in-network referral opportunities
Organizations should review annual MA patient volumes, referral sources, and affiliation percentages to transform abstract data into actionable intelligence, helping care networks intervene earlier and more effectively.
 Strengthening Relationships Using Strategic Insights
Strengthening Relationships Using Strategic Insights
Data-backed transparency into referral flows empowers organizations to take a more nuanced approach to network management. This includes:
- Reinforcing high-performing relationships with providers who consistently refer within the network
- Identifying and engaging underperforming referral sources, where patients may be leaking due to gaps in communication, access, or awareness
- Aligning with MA payer strategies by understanding which providers treat target populations and how they connect patients across the continuum
By illuminating the affiliations between physicians, hospitals, and post-acute organizations, leaders can take a more targeted approach to relationship-building and strategic outreach.
Measuring Progress and Preventing Future Leakage
The true measure of success lies not only in reducing current leakage but in preventing future losses. Leading organizations are establishing continuous feedback loops by:
- Monitoring referral retention rates over time
- Tracking patient volumes by MA payer and provider
- Comparing referral behavior pre- and post-intervention
By leveraging quarterly data updates and payer-level analytics, strategic leaders can adapt more quickly to shifting market conditions, maintain alignment with value-based care goals, and ensure that high-value MA patients remain within the preferred network.
Conclusion
Referral leakage in the Medicare Advantage space represents both a challenge and an opportunity. As MA enrollment grows and competitive pressure intensifies, the ability to monitor, understand, and act on referral trends becomes a defining factor in organizational performance.
With the release of its latest Medicare Advantage dataset, Trella Health is equipping healthcare leaders with the tools needed to turn leakage into loyalty — through data-driven decision-making, stronger referral partnerships, and a deeper understanding of how patients move across today’s complex care landscape.
















