Jess Chew, GM, PAC Provider Growth
With more than 10 years’ experience in healthcare marketing, Jessica not only leads our marketing team but is also a passionate advocate and frequent user of our marketing intelligence solutions. After graduating from the University of Georgia with a bachelor’s in journalism, Jessica got her start in marketing at Gannett, the largest newspaper publisher in America. She thought this entry-level job was the first step on the road to a career as an investigative reporter — but immediately became hooked on marketing. At Trella Health, she’s able to do all the things she loved about journalism — digging for information and insights, helping people share their stories — and she’s also able to make a meaningful difference in the way post-acute care is provided.2021 Skilled Nursing Outlook
OVERCOMING THE CHAOS OF COVID-19
By Jess Chew | January 21, 2021
”We have had more than 50 patients die, both shorter term rehab patients and long-term care residents.”
Those are the words of Jennifer Bishop,* director of rehabilitation for a 170-bed skilled nursing and rehabilitation facility in Massachusetts, reflecting on the human tragedy of COVID-19 in 2020 in skilled nursing facilities.
It’s a sobering reminder that as numb as perhaps we’ve become to the reports of case counts and hospitalizations, the real human toll of COVID has been devastating in our healthcare facilities. The pandemic has uniquely upended and traumatized skilled nursing facilities and their dedicated teams of caregivers, with disruption that has forever changed how SNFs operate.
The New Reality for SNF Patient Care, Staffing, and Census
“I had four staff members from therapy quit because they didn’t want to treat COVID patients,” said Bishop. “Nursing has lost nurses and CNAs. I think every department has had at least one person quit.”
“When a patient is admitted, they spend 14 days in quarantine on our rehab unit. They cannot cohort or share rooms. After 14 days, they move upstairs to continue rehab and that bed becomes available for a new admission.”
The new protocols and changes in patient movement among hospitals and other providers have driven census down. Bishop compares the same day in November 2019 and November 2020:
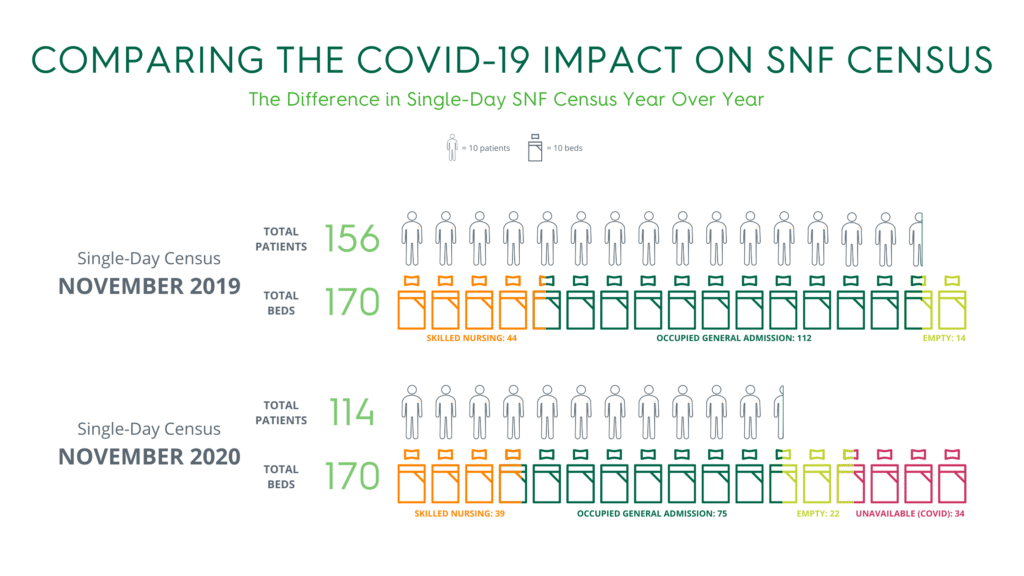
- 2019: Census was 156 with 44 skilled beds. Beds were on hold, awaiting scheduled patients and ready on every unit, and the facility admitted six new patients over the next two days.
- 2020: Census was 114 with 39 skilled. Twenty-two empty beds, with an additional 34 beds unusable because of quarantine restrictions.
This corresponds with recent SNF utilization analysis published by Trella Health, which showed a steep decline from 2018 and 2019 in Q2 of 2020.
Bishop says the facility is also seeing fewer rehab patients and post-elective surgery patients.
“We usually have more elective surgical patients like hip and knee replacements or laminectomies, but elective surgeries are on hold and the ones that do have surgery often go straight home,” she said.
She also describes the current role of the liaisons as constant triage more than proactive referral and relationship management. “Their jobs are very challenging right now. We had to suspend admissions several times due to positive COVID cases and we are currently bed locked until we can move rehab patients off the quarantine unit. Their hands are tied because of bed availability and sometimes nursing staffing issues. They do a lot of bed management and complex negotiations that rival the United Nations.”
The Challenges and Promises of a Post-COVID Future for SNFs
In a recent interview with Skilled Nursing News, Consulate Health Care COO Tim Lehner shared the emphatic immediate focus for the 50-plus facility provider remains staff and patients’ health and well-being.
“There’s nothing in my day more important than making sure that my staff have the tools to be successful, and that the patients are getting what they need and safe in this environment.” he said, further praising front-line caregivers for their heroism in the pandemic.
Given the struggles throughout 2020, SNF leaders maintain some hope and vision while acknowledging the serious challenges they face.
“What are we going to do? You know, even though we’re still in crisis, we’ve already begun that process here,” Lehner said. He notes that Consulate is focusing on workforce, business development, emergency preparedness, and telehealth as priorities both during and after the pandemic.
“One of the things that COVID-19 has really reinforced for me, is that our frontline caregivers — number one, they’re heroes.”
– Tim Lehner, COO, Consulate Health Care
Both Bishop and Lehner were extremely positive about the transition to PDPM for better aligning reimbursements with care and better patient outcomes. They also think the difficult pandemic experience will create some positive behaviors related to infection controls and use of PPE.
Lehner also cites the importance of good data as a guidepost that has given Consulate confidence in their performance in the communities they serve during the COVID pandemic.
As SNF leaders map out their post-pandemic approach, they must grasp data trends, performance, and patient movement across the continuum. What will the patient mix look like and where will those patient referrals be coming from? How will SNFs assess—and impress—the best partner providers and networks for accountable care? Trusted data will help SNF operators stabilize operations and provide the absolute best post-acute skilled nursing and rehabilitative care to those in their communities.
Trella continues to lead in COVID-19 provider insights and analytics for SNFs and across the continuum. This blog continues to provide update COVID-19 perspectives, and look for Trella’s annual Industry Trend Report in January 2021 for more analyses from the most recent Medicare claims data available.
*We have changed Jennifer’s name and slightly altered the facility bed count and census numbers to maintain their anonymity.