Carter Bakkum, Senior Data Analyst, Healthcare Insights
Carter is a senior data analyst who works to turn complex, messy data into actionable intelligence. Carter studied economics and statistics at the University of Virginia before joining an economic consulting firm, where he supported expert testifying economic witnesses on behalf of fortune 500 healthcare companies. After the significant changes in the importance of data analytics during the pandemic, Carter joined the Trella team to dive deeper into the numbers to uncover the stories that drive our experience.Identifying Post-Acute Care Gaps Through Patient Pathway Analyses
By Carter Bakkum | September 30, 2021
What can we learn from studying patient care pathways? By tracking and analyzing the services patients receive starting at a given point in their care journey, we can get a picture of the patient’s care as a whole, and identify any gaps or opportunities to reduce costs and improve care quality. And, while individual patient pathways are helpful, aggregate pathways can do even more. They’re extremely helpful in calculating the utilization of certain services and identifying patient populations that may be underutilizing certain care settings.
To succeed under value-based payment models, it is essential for post-acute care businesses to understand typical patient pathways after an inpatient stay. These populations make up the majority of post-acute care patients and therefore represent the greatest opportunities to increase savings while better serving patients.
Methodology
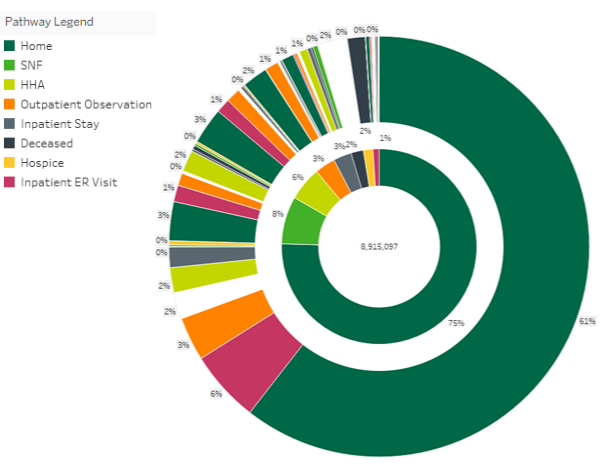
Using access to 100% of Medicare Part A and B claims data, Trella has followed the care pathways of patients after nearly 9 million inpatient discharges in 2020 to gain an understanding of care settings, costs, and outcomes. For this article, we explored care pathways for a large segment of Medicare fee-for-service (FFS) patients, and we then further segmented the data to isolate and analyze high-acuity patient populations.
Medicare FFS patient pathways
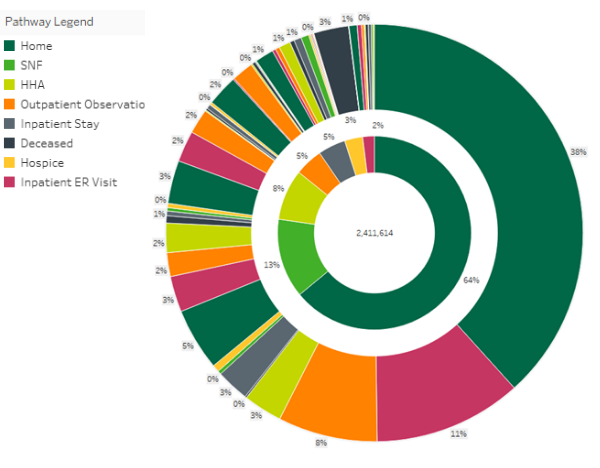
In the first sunburst chart below, we see an illustration of the patient pathways for all Medicare FFS beneficiaries discharged from an inpatient stay at a facility with more than 100 discharges in 2020. The center of the chart illustrates the total number of discharges, and each color indicates the first place of care after an inpatient stay. The outer ring illustrates the second care setting depending on the initial post-discharge care depicted in the inner ring.
Here, we can see that only 8% of total inpatient discharges entered skilled nursing facility (SNF) care within two days of inpatient discharge, and only 1% of total inpatient discharges entered a SNF care setting followed by an inpatient ER setting. As we consider these results, we should also note that, due to suppression requirements from CMS, some patient pathways are unknown. These are illustrated here in white.
The most surprising finding in this analysis is that 75% of discharges are sent home with no post-acute care. Of the patients discharged home (regardless of instruction), 13.8% of them are then admitted to an inpatient stay, emergency room, or outpatient observation center. These beneficiaries represent a substantial opportunity for post-acute care agencies, as nearly 1 million people discharged home without post-acute instructions were admitted to a higher-cost care setting, compared with a home health or skilled nursing facility.
Also of interest, almost 140,000 patients who were discharged home with no post-acute care instructions died without entering hospice care. While it is unlikely that all of these beneficiaries were appropriate for hospice care, there is almost certainly a large portion for whom hospice care would have improved their quality of life in their last days.
Further analysis: High-acuity patient pathways
While the above findings are alarming on their own, deeper analysis of high-acuity beneficiaries discharged from an inpatient stay is even more jarring. For the sunburst chart below, we limited our data to high-acuity beneficiaries, dropping the total population down to 2.4 million discharges. Nearly two-thirds of these high-acuity discharges were released home, and a shocking 30% of these patients were readmitted for an inpatient stay, emergency room, or outpatient observation center.
By further segmenting the available data to analyze these patient populations, post-acute care providers can attain a better understanding of the gaps in the care continuum for their patient populations. SNFs, home health agencies, and hospices can have a significant positive impact on care quality and healthcare costs. Access to this deep level of analysis can help post-acute care providers identify areas where they can fill care gaps, and where they stand out from competing organizations. Further, by sharing this type of data with potential referral partners, show them how healthy referral partnerships can improve care coordination to better serve patients, decrease healthcare costs, and improve business.
Next steps: Appropriate post-acute care is essential to value-based care success
Understanding when post-acute care is appropriate is essential in a value-based care system, as some of the most expensive inpatient stays can be avoided by appropriate utilization of these services. The quality of life and quality of care for these patients can also be exponentially improved by understanding the best care setting to enter after an inpatient discharge.
Trella Health is the leader in market intelligence for the 65+ population, with extensive data sets including Medicare FFS, Medicare Advantage, commercial payers, ACOs, and DCEs. For more insights into how to stand out as a preferred referral partner, schedule a demo today.