Kirsten Reed, Director of Product Marketing
Kirsten is a product marketer who works to surface insights using qualitative and quantitative information. She often refers to her job as a markeologist, part marketer and part archaeologist. Kirsten studied political science at the University of Oregon before beginning her career as a consultant for military intelligence and security clients, where she focused on enabling clients through strategic planning and organizational improvement projects. After receiving her MBA from Emory’s Goizueta Business School, Kirsten transitioned to product marketing. She previously worked in the FinTech space before joining the Trella team. At Trella, Kirsten enjoys the range of activities her role entails, from crafting Go-to-Market messaging to understanding and communicating the nuances of our metrics.Top Takeaways from Health Care Value Week
By Kirsten Reed | March 1, 2022
Trella Health was one of the sponsors for 2022’s Health Care Value Week, which celebrated the significant progress value-based care models have made in addressing health care challenges.
I had the opportunity to join sessions of the Special Edition of the Virtual Value-Based Payment Summit and the NAACOS webinar, “How ACOs Improve Patient Outcomes: Lessons Learned After a Decade of Clinical Transformation.”
Not only did speakers share relevant data points and quantify cost savings alternative payment models (APMs) have delivered, but many also expressed their support for value-based care (VBC) with compelling quotes. Stephanie Quinn of the American Academy of Family Physicians didn’t mince words when she called fee-for-service (FFS) “hostile to prevention and wellness.” Talk about taking a stance!
Here are a few of my top takeaways from the sessions I attended:
Explaining value-based care doesn’t have to be complicated. Aledade CEO Farzad Mostashari, MD shared his definition of VBC as making it more profitable to prevent a stroke rather than treat a stroke. I thought that was a perfect way to sum up what can be a complex concept, one that’s often bogged down with technical details and industry jargon. Melanie Matthews, president of MultiCare Connected Care was similarly straightforward, stating, “FFS is a sick care model whereas APMs offer a health care model.” VBC leaders should employ these types of clear, impactful explanations when looking to gin up support for the transition to value.
Words and terminology matter when it comes to patients buying in. Speaking of industry jargon, Pauline Lapin from the CMS Innovation Center addressed concerns that terms such as “accountable care” and “risk-based” can have negative connotations for patients. “We need to reassure beneficiaries that accountable care isn’t intended to reduce patient choice,” Lapin stated. Terminology also proved to be an issue for the Global and Professional Direct Contracting (GPDC) model. “Direct Contracting Entity” describes the legal structure of a participating organization yet fails to convey anything useful to beneficiaries and comes across as mumbo jumbo. Fortunately, CMS ditched the legalese and chose a more intuitive name for the redesigned ACO Realizing Equity, Access, and Community Health (REACH) Model.
CMS’s three major focuses for value-based care models, alignment, growth, and equity, reinforce each other. In a smart and undoubtedly intentional move by CMS, the focus areas are linked, so that making progress towards one also strengthens another leg of the triangle. For example, VBC organizations providing care to underserved patients in rural areas advance equity while driving growth for their organization. And aligning all payers around value-based care creates additional incentives for smaller practices to join APMs, increasing the number of beneficiaries in an accountable care arrangement.
Learning from setbacks and increasing engagement are crucial for accelerating the transition to value-based care. While the presenters and panelists at times expressed differing opinions and approaches, all agreed the current state of value-based care initiatives leaves room for improvement. Amid highlighting the progress made to date, many speakers also acknowledged the very real challenges healthcare organizations face in the move from volume to value. Challenges cited with APMs included overlapping payment models, complex and unsustainable benchmarks, and barriers to provider participation such as capital and access. The GPDC model was specifically called out, especially the confusion caused when CMS paused the Geo Model less than three months after it was announced. To its credit, CMS continues to incorporate stakeholder feedback, encouraging patients and providers to share the experiences they’ve had with APMs to inform future improvements. Replacing GPDC with ACO REACH, announced February 24, is a very recent example of CMS building on a model, taking the parts that worked well, and refining those that didn’t.
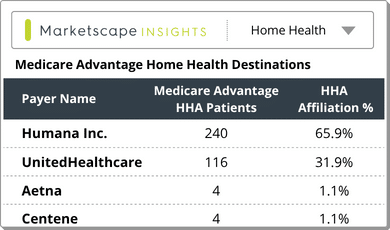
Trella Health is the leader in market intelligence for the 65+ population, with extensive data sets including Medicare FFS, Medicare Advantage, commercial payers, ACOs, and DCEs. For more insights into how to stand out as a preferred referral partner, schedule a demo today.