Carter Bakkum, Senior Data Analyst, Healthcare Insights
Carter is a senior data analyst who works to turn complex, messy data into actionable intelligence. Carter studied economics and statistics at the University of Virginia before joining an economic consulting firm, where he supported expert testifying economic witnesses on behalf of fortune 500 healthcare companies. After the significant changes in the importance of data analytics during the pandemic, Carter joined the Trella team to dive deeper into the numbers to uncover the stories that drive our experience.Patient Care Pathways: Hidden Opportunities for Post-Acute Care Agencies
By Carter Bakkum | December 9, 2021
A patient care pathway illustrates the places of care a patient follows from a given starting point. For our purposes, we chose to follow patients’ care journeys after discharge from an inpatient stay. By analyzing aggregate patient pathways, we can begin to calculate utilization of certain services and identify patient populations that may be underutilizing care settings.
In a value-based care system, acute and post-acute care organizations’ reimbursements (or financial penalties) are largely determined by performance benchmarks, such as cost and quality of care. Thus, it is essential that post-acute care businesses understand typical patient pathways after an inpatient stay, as patients discharged from these acute care settings make up the majority of their census.
Methodology
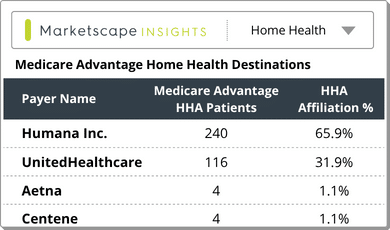
Using access to 100% of Medicare Part A and B claims data, Trella has followed the patient care pathways of nearly 1.6 million cardiac inpatient discharges and 666,000 respiratory patients to understand where Medicare beneficiaries are receiving care after an inpatient stay in 2020. For this analysis, cardiac and respiratory patients were determined based on the International Classification of Diseases (ICD-10) codes and aggregated based on similar diagnoses that align with an organ system or related medical specialty. You can find more information on how the Trella team identified patients for our analysis here.
Tracking patient pathways for circulatory system-related diagnoses
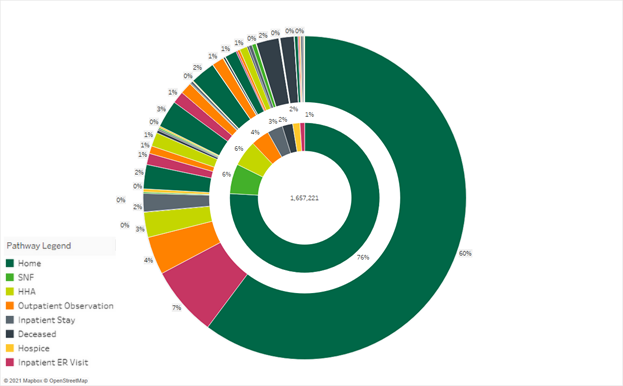
Below is a sunburst chart illustrating the patient pathways for Medicare fee-for-service (FFS) beneficiaries with a primary diagnosis of circulatory system, discharged from an inpatient stay at a facility with more than 100 discharges in 2020. The center of the chart illustrates the total number of discharges, and each color indicates the first place of care after an inpatient stay. The second layer illustrates the second place of care, depending on the initial layer.
1.2 million cardiac patients were discharged home with no post-acute care instructions and spent at least two days at home. Of these, more than 209,000 (16.6%) were readmitted to an acute setting in an outpatient observation center, an inpatient stay, or a visit to an emergency room.
This data represents a potentially massive opportunity for post-acute care agencies, given the extremely high costs associated with inpatient and outpatient care. With this data, we can see that a significant number of cardiac patients are at risk of readmission. By identifying these at-risk populations and partnering with hospitals and health systems, post-acute care agencies can potentially increase their business while improving outcomes and lowering overall costs to patients and payers.
We should note that, due to suppression requirements from CMS, the data here is not complete and some patient pathways are unknown. We have thus excluded these unknown patient pathways from our analysis. However, while this exclusion biases the results toward larger hospital systems, we have seen no indication that the patients sent home without post-acute care recovered from their inpatient stay.
Despite excluded cases, this analysis still indicates that post-acute care organizations, specifically SNFs and home health agencies, have an opportunity to target beneficiaries with circulatory system-related diagnoses to improve patient outcomes and lower costs.
Analyzing patient care pathways for respiratory diagnoses
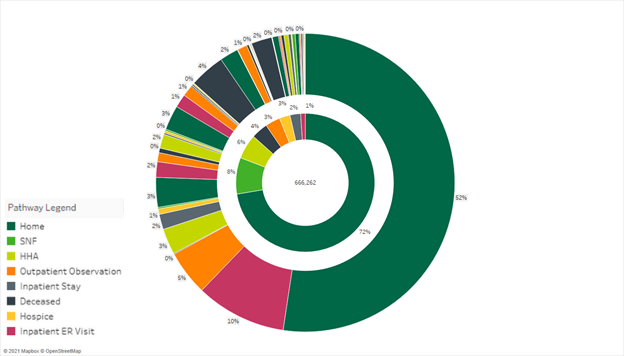
Below, we have a similar sunburst diagram limited to beneficiaries with a respiratory-related diagnosis. As such, the total population analyzed is reduced to 666,262 discharges. The situation here is similar, and perhaps even a bit bleaker. Of the 666,262 discharges, nearly 75% were discharged home with no post-acute care instructions, and a shocking 23% of those patients ended up back in an inpatient stay, emergency room, or outpatient observation center.
By zeroing in on the care pathways of patients with respiratory diagnoses, post-acute care organizations can identify key beneficiaries whose quality of care could be improved with a more appropriate care setting. And, while this data can help post-acute care agencies better serve respiratory patients at any time, it is especially relevant now, as COVID-19 is deadlier to patients with respiratory-related comorbidities. It’s more essential than ever to ensure that these patients receive appropriate care in the right setting.
Further, understanding when post-acute care is appropriate – and in what setting – is essential under value-based payment models. With this information, the most expensive inpatient stays can often be avoided by appropriate utilization of these services. And the quality of life and quality of care for these patients can also be exponentially improved by understanding the best care setting to enter after an inpatient discharge.
Next steps: Demonstrate value with key data on at-risk populations
While improving quality of care has always been the goal, in a value-based care system, that goal is more important than ever. By exploring the patient care pathways of your organization’s core patient populations, you can gain insight into the value you bring to your referral partners. This data can help you demonstrate to hospitals and health systems that discharging appropriate patients to your facility could significantly improve care quality and patient outcomes while dramatically reducing care costs.
Trella Health is the leader in market intelligence for the 65+ population, with extensive data sets including Medicare FFS, Medicare Advantage, commercial payers, ACOs, and DCEs. For more insights into how to stand out as a preferred referral partner, schedule a demo today.